Are Corticosteroid Injections Doing More Harm Than Good?
Jul 11, 2025
Corticosteroid injections are often marketed as a fast and effective way to reduce pain and inflammation. For people suffering from tendon or joint pain, it sounds like a miracle fix.
One quick shot and the pain disappears. But what if this short-term relief comes at the cost of long-term healing—and possibly permanent damage?
That’s exactly what a major review published in The Lancet in 2010 revealed. The researchers analyzed data from 41 high-quality randomized trials, including over 2,500 patients with tendon injuries. What they found should have changed how we approach pain treatment—but unfortunately, it didn’t.
Yes, It Reduces Pain—But That’s Not the Whole Story
Cortisone injections did deliver quick and significant pain relief when compared to doing nothing or even undergoing physical therapy. But here’s the catch: the relief came from suppressing inflammation and pain signals, not from healing the underlying issue. In fact, the review showed that these injections interfered with the body’s natural healing process—delaying recovery and in some cases, causing outright harm. In one trial, a patient experienced a tendon rupture following the injection.
Worse Long-Term Outcomes Than Doing Nothing
At the 6- and 12-month marks, the story took a dramatic turn. Patients who received cortisone injections had:
- A much lower rate of full recovery than those who received no treatment at all.
- A 63% higher risk of relapse compared to those who followed a wait-and-see approach.
- Worse outcomes than patients who underwent physical therapy.
Let that sink in: people who did nothing actually fared better than those who got injections.
And people receiving multiple injections may be at particularly high risk for continuing damage. In one study that the researchers reviewed, an average of four injections resulted in a 57 percent worse outcome when compared to one injection. (Coombes et al., 2010)
The Elephant: Pain Doesn’t Mean Structural Damage

Now here is the big elephant in the treatment room.
One of the most misleading assumptions in mainstream orthopedic medicine is that pain in the area of a tendon means the tendon itself is damaged or inflamed.
This belief is the foundation for both tendinopathy diagnoses and treatments like corticosteroid injections. But growing evidence suggests this view is both simplistic and often dead wrong.
A 2019 study published in the Journal of Shoulder and Elbow Surgery examined MRI scans of both shoulders in 123 people who had pain in only one shoulder. The results were eye-opening:
- Abnormal MRI findings were common in both the painful and pain-free shoulders.
- Only full-thickness supraspinatus tears and moderate osteoarthritis showed a slightly higher frequency (about 10%) on the painful side.
- Interpretation of the scans varied significantly between the radiologist and orthopedic surgeon.
In other words, MRI-detected “damage” is often found in people with no symptoms at all, and different professionals don’t even agree on what they’re seeing. This challenges the idea that what shows up on a scan is reliably the source of pain (Lewis et al., 2019).
In my clinical experience, this disconnect plays out every day. I’ve treated many clients who were diagnosed with rotator cuff tendinopathy, tennis elbow, Achilles tendinosis, or similar issues. I did nothing that would heal a tendon in a 90 minute bodywork session—but instead treated neuromuscular trigger points in muscles referring pain to the tendon area. The results? Rapid and lasting resolution of pain.
The problem is that trigger point referral mimics the symptoms of tendon damage, and these patterns are rarely considered in standard orthopedic evaluations. So people are misdiagnosed, treated with anti-inflammatory drugs or injections, and sent down a path that ignores the actual cause.
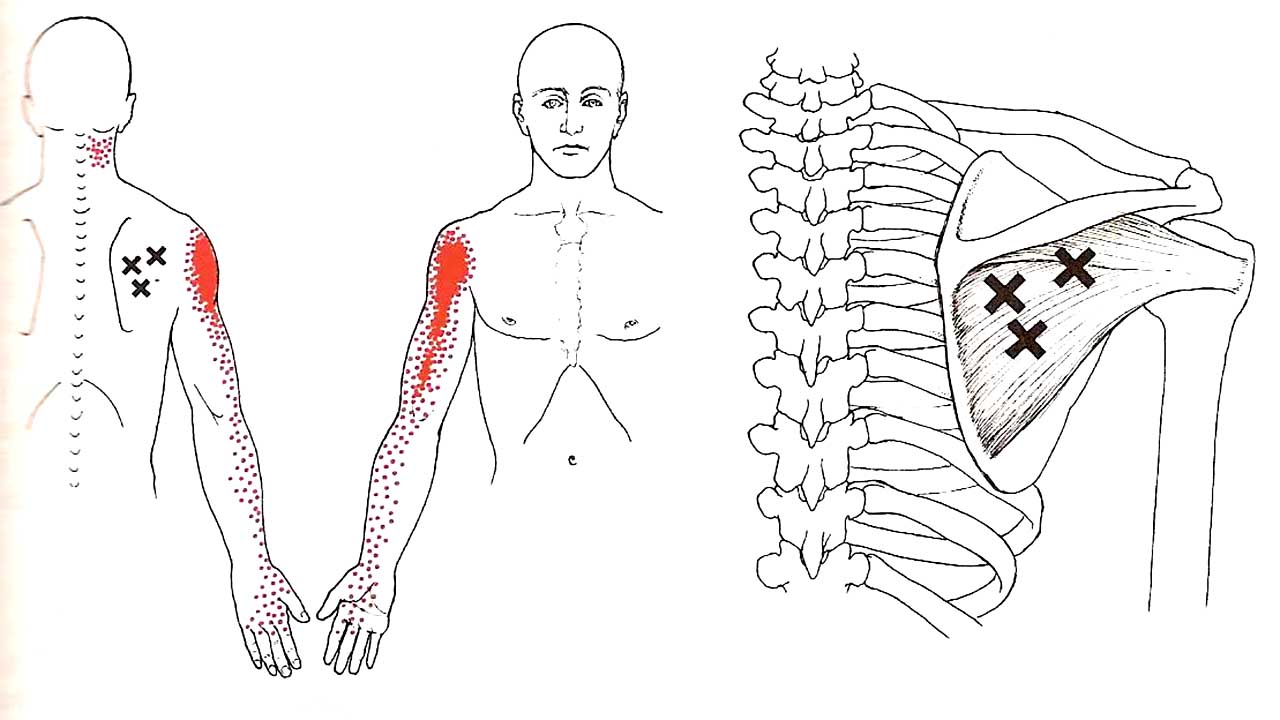
Example: Infraspinatus trigger point referral. X=trigger point, pain referral in red. Often misdiagnosed as bicipital tendinitis because the pain is felt over the biceps tendon.
Most Pain Isn’t What You Think It Is
The assumption that pain always comes from damaged tissue—torn tendons, inflamed joints, or degenerated cartilage—is deeply embedded in both medical thinking and patient belief. But mounting clinical research tells a very different story.
One of the most powerful data points comes from a large observational study published in Advances in Experimental Medicine and Biology (Fogelman et al., 2017). The study examined 997 patients at specialized pain clinics operated by primary care physicians trained in trigger point therapy.
Here’s what they found:
- 82% of patients were diagnosed with myofascial pain syndrome (MPS)—a condition caused by hyperirritable trigger points in skeletal muscles that refer pain to distant areas.
- The majority of these patients reported significant improvement (75%) or complete pain relief after simple treatments like dry needling or manual trigger point therapy.
- These results were achieved without advanced imaging, invasive diagnostics, or surgical intervention—and only 5–6% of patients required referral for imaging or specialist consultation.
In other words, most patients with persistent musculoskeletal pain weren’t suffering from joint or tendon injury at all. Their pain was muscular, referred, and highly responsive to inexpensive, conservative treatment.
This finding aligns with the daily reality I see in my practice: people are often diagnosed with conditions like rotator cuff tendinopathy, Achilles tendonitis, or lateral epicondylitis (tennis elbow) based solely on the location of the pain—and sometimes a scan that shows “degeneration.” But when we treat the actual trigger points in the muscles that refer pain to those areas, the pain resolves—without ever touching the tendon.
This is why relying on injections to calm “inflammation” in a tendon is often a wild goose chase. The pain is usually not coming from the tendon at all.
The Hidden Danger of Local Steroid Injections
When pain is referred from a trigger point in a muscle, but the steroid injection is given at the site where pain is felt—like a tendon or joint—you’re doing two harmful things at once:
- You’re missing the true source of the problem.
The pain may be coming from a distant muscle, but you’re injecting the symptom, not the source. - You’re damaging local tissue that wasn’t the cause to begin with.
Corticosteroids suppress healing, weaken collagen, and increase the risk of rupture in tendons and joint structures. So now you’ve created a weaker tissue environment, but the pain driver is still active somewhere else.
This is like silencing a fire alarm in the bedroom when the fire is actually in the kitchen—and pouring water on your bed in the process.

A Better Way Forward
Instead of suppressing the pain response, we need to listen to it. When we investigate where pain really comes from—most often referred from muscles, not the site of the pain experience—we can actually resolve the root problem.
That’s what we do through trigger point therapy and retraining pain-free movement in Coaching The Body® methodology. We don’t suppress symptoms, but offer something better: real healing.
References
- Coombes, B. K., Bisset, L., & Vicenzino, B. (2010). Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: a systematic review of randomized controlled trials. The Lancet, 376(9754), 1751–1767. https://doi.org/10.1016/S0140-6736(10)61160-9
- Lewis, J. S., Green, A., & Dekel, S. (2019). Abnormal findings on shoulder MRI are common in both symptomatic and asymptomatic individuals. Journal of Shoulder and Elbow Surgery, 28(8), 1533–1540. https://pubmed.ncbi.nlm.nih.gov/31279721/
- Fogelman, Y., Carmeli, E., Minerbi, A., Harash, B., & Vulfsons, S. (2017). Specialized Pain Clinics in Primary Care: Common Diagnoses, Referral Patterns and Clinical Outcomes – Novel Pain Management Model. Advances in Experimental Medicine and Biology, 1047, 1–12. https://doi.org/10.1007/5584_2017_108



